Introduction |
Leiomyosarcoma (LMS) is one of the most common subtypes of soft tissue sarcoma (STS) and accounts for approximately 24%, LMS start from cells in a type of muscle tissue called smooth muscle or involuntary muscles - the brain has no conscious controlover them. They can be found in the walls of muscular organs like the heart and stomach, as well as in the walls of blood vessels throughout the body. Even though LMS are most common in the uterus, abdomen or pelvis, they can basically start anywhere in the body. Even though the histology of the tumours is similar, soft tissue leiomyosarcoma can be subdivided into four groups: LMS of retroperitoneum and abdominal cavity, LMS of somatic soft tissue, cutaneous LMS, LMS of vascular origin. This subdivision has an impact on treatment and can give hints on prognosis. LMS can also occur in the bones – however, this is very rare. Most people are over the age of 50 years when diagnosed with LMS with more women affected than men (2:1). It is not clear why leiomyosarcomas develop. However, some risk factors are known: previous radiotherapy, some rare hereditary syndromes and exposure to some types of chemicals, including vinyl chloride, some types of herbicides and dioxins. |
Signs and symptoms |
There are no symptoms specific to leiomyosarcomas. However, an abdominal mass or swelling, pain, weight loss, nausea or vomiting can occur. This is often the case for leiomyosarcomas of the retroperitoneum. In contrast, leiomyosarcomas of the somatic soft tissue often present as enlarging, painless mass and LMS of major blood vessels can lead to (among other symptoms) leg edema or numbness from compression of nearby nerves. |
Diagnosis |
When a sarcoma is suspected, the first step is the evaluation of the patient’s medical history and a thorough clinical examination. However, when a lump is present, imaging tests are important to assist with diagnosis and so-called staging. Several diagnostic methods will be applied:
|
Treatment |
The treatment of soft-tissue sarcomas including leiomyosarcomas should be performed in a sarcoma centre. It is usually "multi-modal". This simply means that different therapy modalities are combined in incremental, alternating, and sometimes simultaneous ways. The planning of a treatment strategy starts with a review of the patient’s history, all available imaging, and the pathologic results from biopsy. On this basis, a multi-disciplinary team of surgeons, oncologists, radiologists, pathologists etc. discusses treatment options and comes up with a treatment plan which depends on several factors such as primary tumour location, extent of the primary tumour (stage), degree of malignancy (grade) and the existence of metastasis. Surgery The main form of treatment for leiomyosarcomas is surgery with the aim to remove the entire tumor and surrounding tissue (wide margins). Whether this is possible or not depends on size, location and spread of a tumor. Radiation therapy Some tumours involve or are very close to vital structures. In these cases, surgery of the tumour with wide surgical margins is not possible. Radiation therapy can then be applied in order to shrink the tumour and turn it operable (neo-adjuvant treatment). It can also be an option after surgery, in order to avoid either local or regional recurrences, which may develop from microscopic cells left over after surgery. If the disease has already spread, radiation therapy can be utilized as a means of palliative local control. Chemotherapy Chemotherapy can be an option if the disease is locally advanced, metastatic, or recurrent, possibly in combination with surgery and/or radiation therapy. It is quite common that multiple chemotherapies are applied (combination therapy) or they can be used sequentially. Agents currently used for the treatment of LMS are doxorubicin and ifosfamide, gemcitabine and taxotere (docetaxel), dacarbazine, pazopanib and trabectedin. In 2015, a novel type of chemotherapy – trabectedin (Yondelis®) – was approved by the FDA (Food and Drug Administration, the US medicines agency) for leiomyosarcoma (and liposarcoma) that cannot be removed by surgery or for patients that previously underwent treatment that contained anthracycline (specific type of chemotherapy). As LMS are so rare, there are currently no standard or overall effective type of chemotherapy or radiation and the optimal use of chemotherapy and radiation continues to be evaluated. |
Follow-Up |
If all demonstrable disease is removed, then there will be follow up examinations. They usually include CT scans of chest, abdomen and pelvis every three months for two years, then every six months for another three years, then yearly. Some centers do ultrasound abdomen & pelvis and chest Xray instead of the CT scans, or alternating with them. |
Research |
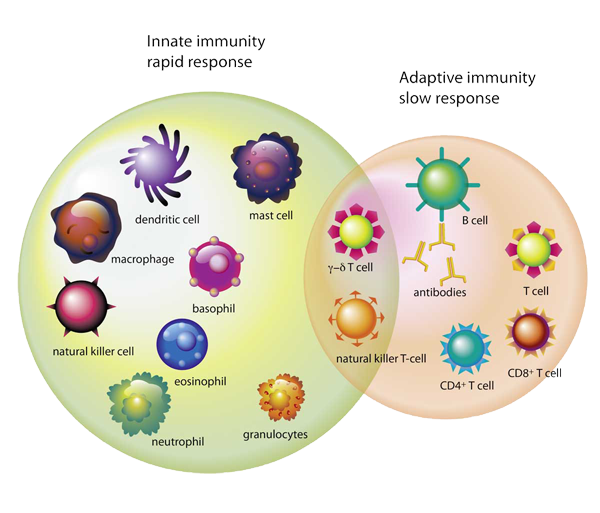
New treatments for soft tissue sarcomas are currently being tested in clinical trials. These include new chemotherapeutic drugs (and combinations), but also so-called angiogenesis inhibitors (prevent the formation of new blood vessels needed to supply tumours) and immuno-oncology agents that reactivate the immune system to fight cancer cells. |
A very special thanks to Dr. Robin Jones, UK for medical proofreading!